History of Psychiatry at the University of Utah School of Medicine
By David A. Tomb, M.D.
The Department of Psychiatry’s contribution to the private, public, and academic practice of psychiatry in Utah is long and rich, dating from almost the inception of the School of Medicine.
Many of the private psychiatrists throughout the state have graduated from the University’s program. Others maintain clinical faculty positions, benefiting both the department and themselves. Moreover, the Department of Psychiatry has long provided a variety of CME activities, such as the Psychiatric Grand Rounds, for the professional community at large, thus helping all psychiatric practitioners in their never-ending effort to stay current.
Equally important, the Department of Psychiatry has played a central role in the development of the Community Mental Health (CMH) Centers throughout the state. Several autonomous rural psychiatric clinics had been established by department faculty members before the onset of the Federally sponsored CMH movement. They helped serve as models for those centers that were developed later with federal, state, and county support. In addition, most of the psychiatrists who have staffed these centers over the years have come either directly as psychiatry residents or indirectly as graduates of the Department of Psychiatry training program. The department has provided consultative aid to many of these centers during their growing phases and continues such aid today in selected cases. Finally, the core psychiatric inpatient care delivered by the largest of these centers, the Salt Lake Community Mental Health Center, is provided on one of the psychiatric wards at the University Hospital by psychiatric residents and department faculty.
The final goal of the Department of Psychiatry is academic: training and research. No medical student is graduated from the University of Utah without exposure to classroom, hospital ward, and clinical psychiatry provided by department faculty. It has been that way since the beginning of the School of Medicine, and presumably, will so remain. Likewise approximately 2 to 4 residents in adult psychiatry and 1 to 2 fellows in child psychiatry have graduated each year for two decades. The residency program continues to gain in stature nationally, as reflected by an ever increasing number of applicants. This year 40 applicants were interviewed for the five available first-year training slots. Currently, there are 27 residents in various stages of training.
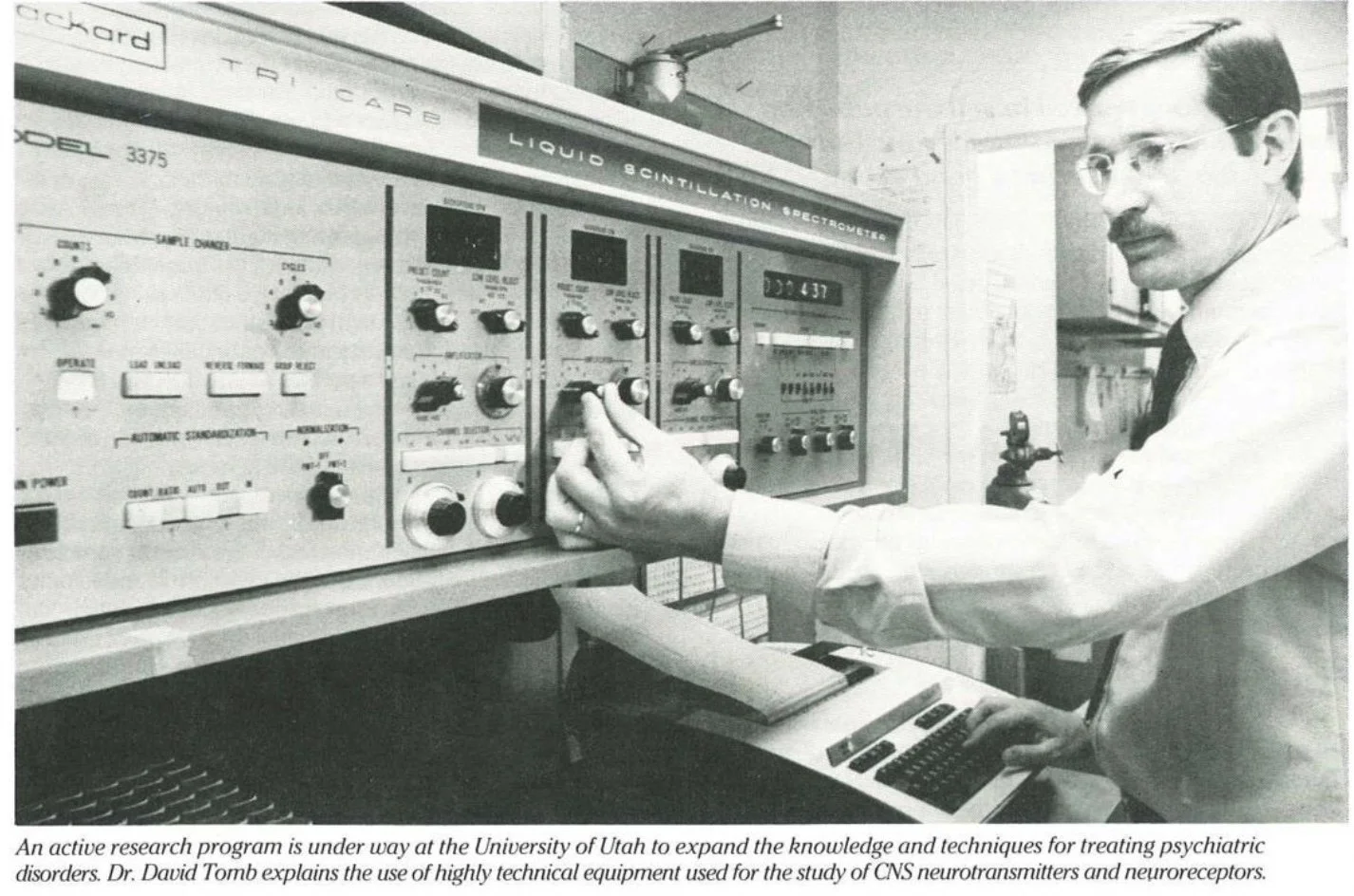
Research, particularly biological research, has been a “raison d’etre” for the department for many years: from the past experiments of Dr. Lincoln Clark on the effects of psychedelic substances on monkeys and the endocrinological investigations of Dr. Eugene Bliss, to current studies on the effectiveness of new antidepressant drugs, the neurobiology of Central Nervous System (CNS) neurotransmitters, evaluation of childhood methods for treating chronic pain, the nature of childhood hyperactivity
(Attention Deficit Disorder) as it manifests itself in adults, and the etiology and treatment of that curious (but fairly common) syndrome known as the multiple personality.
Clinical services provided by the department of psychiatry
Clinical services at the University Hospital are built around two inpatient wards: a 28 bed open/closed unit and a separate 20 bed open ward. Each ward carries a full complement of faculty, nurses, social workers, recreational therapists, and other professionals as well as psychiatric residents and a variety of trainees from other professional disciplines. The larger ward serves as the inpatient service for the Salt Lake Mental Health Center and also receives from private sources some of the most seriously psychi- atrically ill patients in the community. The smaller ward treats many special populations such as those from behavior medicine and those who are eating disordered, phobic, anxious, depressed, etc.
The School of Medicine is, of course, closely allied with the Utah Veteran’s Administration Hospital and thus the psychiatric clinical facilities there work in tandem with those at the University Hospital. This includes approximately 120 inpatient beds spread among general psychiatric, substance abuse, and alcoholism populations. Also included are the associated psychiatric outpatient services.
The Department of Psychiatry faculty members all maintain private practices out of their offices within the department. Moreover, several specialty clinics have been established to better address the needs of certain complicated problems:
The Behavior Medicine Clinic 'The Child and Adolescent Depression Clinic The Adult Depressioin Clinic The Anxiety and Phobias Clinic The Eating Disorders Clinic Although each is primarily a private clinic, they all incorporate sophisticated diagnostic protocols and research standards so that the patients seen generate data valuable in directing their own care as well as in helping to answer treatment questions for the clinic population as a whole. This is consonant with one of the department’s primary goals — to so closely ally research and clinical practice that each benefits directly and substantially from the other. Moreover, this structure serves as a model to participating residents as to what good clinical care can be like if practiced thoughtfully and rigorously.
Finally, the Department of Psychiatry is not standing still. New research, clinical, and educational efforts are continually being generated in response to both faculty interest and the needs of the community.
Current research efforts
The Department of Psychiatry is a major center for the investigation of new antidepressant medications. The Depression Research Clinic is directed by the Departmental Chairman, Dr. Bernard Grosser, and has maintained a study population of several hundred seriously depressed adults over the past several years. Because of the noteworthiness of this clinic, the newest and most promising of antidepressant drugs have been made available for study there. Besides Dr. Grosser, research faculty include Drs. Paul Wender, Fred Reimherr, and David Wood. Moreover, the clinic has proven a fertile ground for the training of advanced psychiatric residents in both research methods and the more sophisticated use of antidepressants.
Dr. James Wamsley has created a psychobiology laboratory within the department devoted to the study of CNS neurotransmitters and neuroreceptors primarily in animal models. In over 50 papers produced during the past three years, his studies have dealt primarily with localization of neurotransmitter receptors in normal and pathological states.
The Division of Behavioral Medicine within the Department of Psychiatry has had an active research program for the past ten years in the use of psychiatric/behavioral techniques to supplement traditional medical/pharmacological methods for treating chronic pain syndromes. Their results have been in keeping with those observed nationally. Their studies have added to our general understanding of the mind-body interaction, and they have provided a continuing clinical service to the professional community and its patients.
Dr. Paul Wender, a pioneer in the concept of adult hyperactivity, has studied this population as thoroughly as anyone in the country and has concluded that the condition is not only common but often treatable with stimulant medication.
Dr. Eugene Bliss, although engaged for many years in biological research, has recently turned his attention to the increasingly recognized phenomenon of multiple personality. Using hypnotic techniques for both diagnosis and treatment, he has documented that many of these patients develop this clinical syndrome by means of a self-hypnotic process. People who are naturally (genetically?) good hypnotic subjects seem prone to fall into semi-hypnotic states and to develop additional personalities inadvertently in an effort to protect themselves psychologically during times of stress. Although the limits of the syndrome have not yet been delineated, interest is international; and,Utah’s contribution is well recognized.
Occasional, more limited research efforts are pursued by other faculty members from time to time. Moreover, research by psychiatric residents is encouraged, but, unfortunately, underfunded. In addition, research by department faculty is ongoing in settings other than the School of Medicine. For example, Dr. William McMahon maintains a clinic for research in and treatment of learning disabled children at the Primary Children’s Medical Center.
Finally, several of the focused clinical services of the Department of Psychiatry have an integrated research component, since we are convinced that only by forcing clinical activities to stay current with the latest research will they be able to provide the highest level of care.